 Press
Press
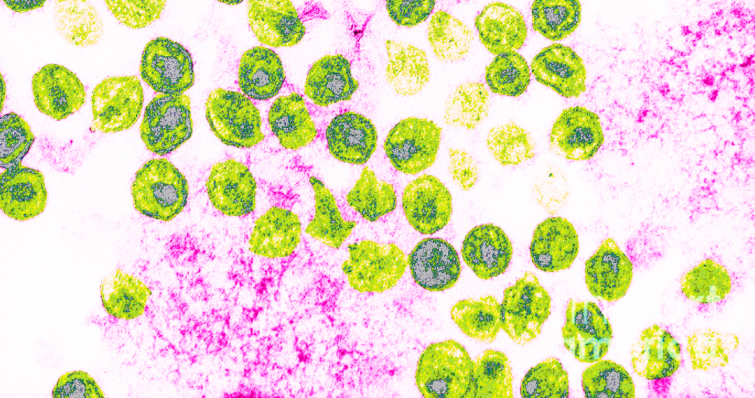
HIV – Examining the immune system in different types of controller patients
1- HIV: The antibodies of "post-treatment controllers"
A very small percentage of people with HIV-1 and who received early treatment maintained over several years have the capacity to control the virus over the long-term when their treatment is interrupted. However, the mechanisms of this control have not been fully elucidated.
The team of researchers, led by Dr. Hugo Mouquet, director of the Laboratory of Humoral Immunology at Institut Pasteur (partner research organization of Université Paris Cité), conducted an exhaustive study in PTCs in order to characterize their humoral response (i.e. their production of B cells and specific antibodies), compared with non-controllers.
The scientists have shown that the humoral immune response profiles vary according to the activity of the virus observed in the subjects.
In PTCs who experience short episodes in which the virus resumes low-level activity after interruption of treatment, transient exposure to the viral antigens induces:
a strong anti-HIV-1 humoral response, involving more frequent intervention of HIV-1 envelope-specific memory B cells;
the production of antibodies with a cross-neutralizing action and which possess "effector" antiviral activities in which the innate immune cells recognize the infected cells bound to the antibodies, thereby inducing their elimination;
the increase in the blood of atypical memory B cells and subpopulations of activated helper T cells.
This specific, multifunctional, and robust humoral response could help to control their infection in the absence of treatment.
However, other PTCs in whom the virus continuously remains undetectable after treatment interruption do not develop a strong humoral response. The control mechanisms in these patients continue to be investigated in the VISCONTI study.
The discovery of these two types of humoral immune response, which depend on the profile of the PTCs, sheds new light on the phenomenon of HIV control. For Dr. Mouquet, researcher at Institut Pasteur and principal investigator of the study, "these findings show that early antiretroviral treatment can facilitate the optimal development of humoral immune responses, in some cases countering viral rebound after treatment interruption." The example of the immune response of the PTCs having short episodes of "awakening" of the virus could even inspire novel therapeutic or vaccine strategies.
2- IgA broadly neutralizing antibodies in HIV-1 natural controllers
Some rare individuals infected with HIV-1 (1%), known as elite neutralizers, develop remarkably effective immunoglobulin G (IgG) antibodies in the absence of treatment. These broadly neutralizing antibodies (bNAbs) target the envelope protein (Env) of the virus and neutralize the majority of HIV-1 viral variants, referred to as quasispecies. Several distinct neutralizing sites recognized by these IgG bNAbs, known as vulnerability sites, have been identified on the HIV-1 Env protein. A protective vaccine should therefore ideally induce broadly neutralizing antibodies. For scientists, understanding the mechanisms of development of these antibodies is a key step towards the aim of inducing their production by vaccination. Considerable efforts have been made to try to design such vaccines, but so far without success.
In a new study, scientists from the Humoral Immunology Laboratory led by Hugo Mouquet, in collaboration with the Structural Virology Unit led by Félix Rey, identified and provided detailed characterization of new bNAbs from three distinct B lymphocyte lineages. For the first time, both IgA bNAbs (the predominant antibodies in the mucosa) and IgG bNAbs were characterized in a viremic controller, in other words an individual who naturally controls infection in the absence of treatment. Drawing on structural analyses using electron cryomicroscopy, the scientists demonstrated that all these bNAbs (IgG and IgA) target the same neutralizing site, known as the N332 "supersite." This demonstrates that individuals controlling HIV-1 infection are able to co-develop several lineages of B lymphocytes producing IgG and IgA bNAbs targeting the same Env vulnerability site. These antibodies could therefore play a role in immune control of the virus. The original results also show that effective IgA bNAbs targeting the N332 supersite are produced in response to HIV-1 infection, with an antibody response maturation signature compatible with the potential response induced by vaccines. The latter characteristic could be essential in blocking mucosal transmission of the virus.
This research was published in the Journal of Experimental Medicine.